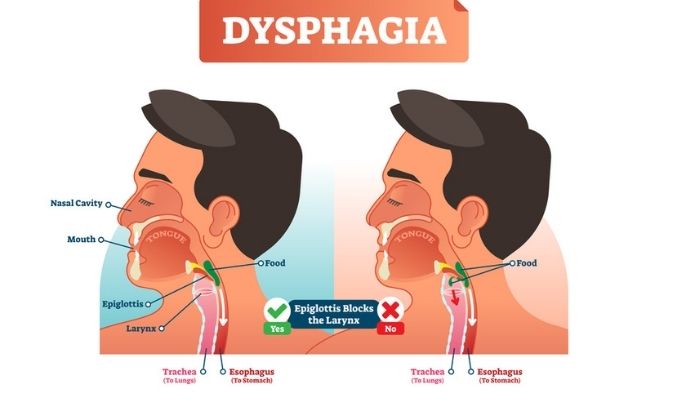
Esophageal Dysmotility, or ED for short, is a condition that causes dysphagia, or difficulty swallowing, causing food to get stuck in your throat. The muscles in the esophagus don’t work well, making it difficult for people with this condition to swallow. They may also have trouble talking or breathing because of the obstruction.
The digestive system helps the body break down the food that we eat and absorbs nutrients into our bodies. It starts in the mouth, passes through the esophagus, stomach, small intestine, and large intestine then ends in the anus.
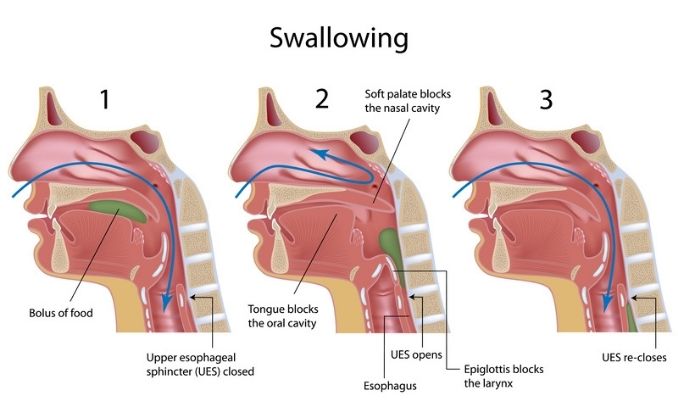
The esophagus is a tubular muscular organ approximately 25cm in length, with an upper esophageal sphincter (UES) made of striated muscles creating a tonically closed valve and preventing air from entering the gastrointestinal system. It also has a lower esophageal sphincter (LES), made of smooth muscle that creates a baseline tone to avoid gastric reflux into the esophagus. There are two layers of esophageal muscles: the inner circular layer, which forms lumen occluding ring contractions, and the outer longitudinal layer, which is responsible for esophageal shortening. These two muscle layers are known collectively as the muscularis propria.
The esophagus delivers food from the mouth to the stomach through esophageal peristalsis. The LES relaxes during swallows until the peristaltic wave travels through it, which contracts and redevelops the resting basal tone. This coordinated, sequential motility pattern propels food from above and clears acid and bile reflux below.
Causes of Esophageal Dysmotility
Primary esophageal motility disorders are idiopathic, a disease that arises spontaneously or for which its cause cannot be determined. Its pathophysiology is poorly defined, except for achalasia which is characterized by the absence of esophageal peristalsis and impaired relaxation of the LES. Secondary esophageal motility disorders manifest as a systemic diseases, including scleroderma esophagus and esophageal motility disorder of diabetes.
Scleroderma Esophagus
Scleroderma esophagus is one of the secondary esophageal motility disorders that scleroderma causes. It is a systemic process causing smooth muscle atrophy and fibrosis. Striated muscles make up the UES, while smooth muscles make up the lower part of the esophagus, including the LES. As fibrosis or scar tissue progressively replaces esophageal smooth muscles, it can gradually lead to progressive loss of peristalsis and weakening of the LES, thus manifesting the signs of esophageal dysmotility.
Signs and Symptoms
- Progressive dysphagia is the hallmark of achalasia. Dysphagia for solids is more common than for liquids.
- A person may be unable to lie in bed if the food accumulated in the dilated proximal esophagus is regurgitated. They must sleep using multiple pillows or upright in a chair with their head elevated at a 30-degree angle. This symptom worsens as the esophagus progressively dilates with time.
- Chest pain squeezes the retrosternal area and radiates to the neck, jaw, arms, or back. This mimics the chest pain of acute coronary syndrome. The chest pain may worsen with food and can awaken patients from sleep.
- A sensation of heartburn is experienced in some patients, assumed to be due to retained food fermentation and lactic acid.
- Gradual weight loss
- Emotional stress or rapid eating may worsen all of the symptoms mentioned above.
Scleroderma Esophagus
Scleroderma involves the esophagus in more than 75% of patients where it may be progressive systemic sclerosis (PSS). It is incorrect to assume that the involvement of other organs is always more severe than esophageal involvement. Calcinosis, Raynaud phenomenon, esophageal dysfunction, sclerodactyly, and telangiectasia are early manifestations of the fulminant form of the disease. Patients with diminished peristalsis or peptic strictures may present with dysphagia as the primary clinical sign. Patients may also experience heartburn and regurgitation. These esophageal symptoms reflect the severity of the acid reflux disease in scleroderma.
Esophageal Dysmotility versus Other Medical Conditions:
Angina Pectoris
An imbalance of myocardial blood supply and oxygen demand causes angina. It is a common presenting symptom among coronary artery disease (CAD) patients.
Compared to esophageal motility disorders, they both present with retrosternal chest discomfort (pressure, heaviness, squeezing, burning, or choking sensation). However, it is excluded because the chest pain in angina pectoris is precipitated by exertion, exposure to cold, or emotional stress and relieved by rest or nitroglycerin. In contrast, the chest pain of esophageal motility disorders may be aggravated by lying flat in bed. Esophageal motility disorders associate with other esophageal symptoms, like a history of progressive dysphagia.
Chagas Disease
Chagas is an infectious disease caused by the protozoan T cruzi, transmitted by a reduviid (kissing) bug bite. This disease is endemic in South and Central America.
Pathophysiology shows widespread ganglionic destruction throughout the body, involving the heart, gastrointestinal tract, urinary tract, and respiratory tract, but the clinically significant disease takes years to develop.
How Is This Diagnosed?
Radiography
With long-standing achalasia, the esophagus, as seen in chest radiography, dilates and exhibits a sigmoid appearance. We observe an air-fluid level, a widened mediastinum, and the absence of a gastric air bubble.
Barium Swallow Test
This imaging test uses barium (the patient swallows the barium) and X-rays to create images of the upper gastrointestinal (GI) tract.
The classic sign is a tapering of the LES, creating the characteristic “bird-beak” appearance in advanced achalasia. Early achalasia would reveal a normal anatomical esophagus with loss of peristalsis and temporary stasis just above the gastroesophageal junction (GEJ), the junction between the stomach and the esophagus.
In patients with scleroderma esophagus, the esophagram shows a slightly dilated esophagus, weak or absent peristalsis, and free reflux.
Endoscopy
Endoscopy is a procedure to visually examine the upper digestive system with a tiny camera on the end of a long, flexible tube inserted through the mouth. It is used to exclude mechanical and inflammatory lesions causing dysmotility symptoms. When considering achalasia, endoscopic evaluation is critical in looking for a structural cause for obstruction.
Treatment
Patients suspected of having esophageal motility disorder need proper evaluation by a gastroenterologist.
In achalasia, we cannot cure the primary underlying neuropathology process; therefore, the primary goal of treatment is symptomatic relief. Treatment goals aim to relieve the physiologic obstruction at the level of the LES by surgical or endoscopic balloon disruption of the LES muscle or, less effectively, through medications that relax the LES smooth muscle.
In patients with scleroderma esophagus, treatment involves aggressive anti-reflux therapy and management of reflux complications like esophageal stricture and dilation.
Botulinum Toxin Injection – Botulinum toxin, one of the most poisonous biological substances known, is a neurotoxin produced by the bacterium Clostridium botulinum. It interferes with neural transmission by blocking the release of acetylcholine, the principal neurotransmitter at the neuromuscular junction, causing muscle paralysis. The weakness induced by injection with botulinum toxin A usually lasts about three months. Botulinum toxin injections into the LES have been used in treating patients with achalasia. The doctor uses a sclerotherapy needle to inject 80-100 units of botulinum toxin into the four quadrants of the LES.
It is a good substitute for patients who are poor surgical candidates, such as elderly patients or frail individuals. However, this treatment is costly, and there is a need for repeated therapeutic sessions because, as mentioned, the weakness induced by botulinum toxin usually lasts for only three months.
Endoscopic Therapy – Esophagogastroduodenoscopy (EGD) with pneumatic dilation is the standard endoscopic therapy for patients with achalasia and can be performed on an outpatient basis. In this procedure, we distend the LES forcefully to 3 cm, disrupting the circular muscle layer, which causes the relative esophageal obstruction for symptomatic relief. Balloon dilators specifically designed for achalasia achieve adequate diameter for lasting effectiveness.
Surgical Care
Surgical treatment targets to disrupt the LES through myotomy, which is the surgical procedure of cutting the esophageal muscle to relieve the high pressures at the gastroesophageal junction. It treats younger and older patients who are good surgical candidates. In severe cases, when there is distortion or malignancy of the esophageal anatomy, esophagostomy, or the removal of a portion of the esophagus, becomes the surgical procedure of choice.
In other forms of esophageal motility disorders, surgeons rarely indicate surgery because these disorders generally are tolerable and do not cause malnutrition or dehydration.
Home Care Program
- Modification of Dietary and Eating Habits
- People prefer smaller, more frequent meals over the larger meals associated with the traditional three meals daily. Liquid foods pass down the esophagus and through the LES with less resistance, so patients should follow food boluses with liquids frequently.
- Take smaller bites of food, with thorough chewing and slow swallowing.
- Swallow only once per bite. Avoid double swallows. Taking a second swallow can diminish esophageal motility. Wait 15 seconds after every swallow before initiating a dual swallow.
- Remain upright during and for some time after mealtime (at least 2 hours) to enhance esophageal emptying.
- Be very careful about taking pills. Pills can take a long time in your esophagus and cause significant damage. Swallow tablets with a large amount of water (12 oz) and remain upright for one hr. after taking them. Try liquid formulations of your medicines if possible.
- Straightening the back, raising arms above your head, and standing can increase intra-esophageal pressure, enhancing esophageal clearance.
Activity
Avoid exercising right after a meal, for it can promote esophageal regurgitation. Avoid lying down during and after mealtime to enhance esophageal emptying and improve symptoms.
You may also benefit from esophagus-strengthening exercises:
1. Chin Dips
Practice chin dips to exercise the esophagus and sphincter at the top of the throat and to facilitate swallowing. For example, drop the chin slightly toward the chest while sipping when drinking or eating small amounts of fluid or food. This enables the epiglottis’s positioning and narrows the throat’s entrance by the trachea or windpipe. This is also an effective remedy for individuals who have trouble swallowing pills and reduces the chance of choking and regurgitation. You can practice this positioning and swallowing exercise several times throughout the day.
2. Suck and Swallow
This exercise strengthens the muscles of the tongue and forces you to concentrate on the strengths and process of swallowing, as well as pulling more saliva to the back portion of the mouth while eating. Practice by gently pressing the tongue to the back of the front teeth. Pull the cheeks in slightly as if you’re trying to suck air from the tip of your tongue to the back of the mouth. You’ll feel a distinct pull along the cheeks, the language’s side, and the throat’s upper part. Then swallow. Repeat this exercise several times a day.
3. Airway Exercises
Strengthen the throat muscles that facilitate swallowing by holding your breath, grasping the sides or arms of a chair, and pulling upward or pushing downward simultaneously. Hold the contraction and your breath for a few seconds, then release. Focus on your throat and if necessary, lift one hand to feel the throat muscles contracting. This may help you focus on isolating and controlling the proper throat muscles for swallowing.
4. Swallowing Exercise with Held Breath
You can practice swallowing exercises while holding your breath to strengthen your throat and sphincter muscles and help prevent choking while drinking and eating. For example, place a small amount of fluid in your mouth and keep it there while holding your breath. Concentrate and then swallow, continuing to hold your breath while you eat. Immediately after ingesting the fluid, cough lightly.
You cannot eat a regular meal like most individuals. If you eat a large meal in one sitting, a significant portion of the food may sit in your esophagus for a very long time. When the food rises up from the esophagus and irritates the throat and lungs, it causes heartburn, cough, and other symptoms. A person with esophageal dysmotility may have serious problems when eating a large meal.
Achalasia
Achalasia is a progressive disease, thus requiring chronic therapy. When advanced, this condition can lead to severe dysphagia, causing malnutrition, weight loss, and dehydration. Even after treatment, patients continue to have mild symptoms of aperistaltic esophagus, so careful eating habits must always be practiced.
Patients with long-standing achalasia also observe an increased incidence of esophageal squamous cells and adenocarcinoma.
Scleroderma esophagus
Scleroderma is a progressive, systemic disease. Systemic complications are the primary cause of mortality.
Significant acid reflux causes disabling symptoms due to the reflux itself or its complications. Associated complications, including strictures, Barrett esophagus, and adenocarcinoma of the esophagus, are the concern.
Your gut is the key to many health concerns. Learn how to better your digestion for better overall health here.